Levelling the Playing Field: Why Care Quality Matters More Than the Next Drug
- Posted:
- Written by:
-
- James Galloway
- Categories:
For two decades, I have been immersed in studying the safety of drugs we prescribe in rheumatology. Over that time, one striking truth has become clear to me. At first, my work focused on comparing the safety of targeted therapies in rheumatoid arthritis - measuring whether the latest monoclonal antibody performed better or worse than another shiny new drug. Methodologically, it was fascinating work, and the differences we identified were real. But when you zoom out, the truth is those differences were often small in real-world terms.
It was only when I started asking different questions, looking not just at which drug was chosen, but at the quality of care patients received across the NHS… that the scale of variation truly hit me.
Beyond the “postcode lottery”
The idea of a “postcode lottery” in healthcare always struck me as a slightly sensationalist headline. But the more I examined regional variations in care, the more undeniable the picture became.
The differences in outcomes associated with how care is delivered dwarfed the differences I had spent years measuring between treatment options. Levelling the playing field, i.e. ensuring more equitable care delivery across the country, could deliver benefits far greater than the marginal gains of drug-to-drug comparisons.
We already have a wealth of effective treatments. The real challenge is not simply inventing the next therapy, but ensuring the drugs we already have are used appropriately, consistently, and safely. And here lies the evidence-practice gap: how do we translate the best prescribing evidence into everyday clinical practice, across the entire country?
Methotrexate: a case study in preventable risk
This brings me to methotrexate, a cornerstone drug in rheumatology. It comes in two tablet strengths: 2.5mg and 10mg, both taken once weekly, usually at a dose of 15-20mg. The risk is obvious: if a patient normally takes 8 × 2.5mg tablets once a week, but is switched to 10mg tablets (which look very similar), they could mistakenly take 80mg -a potentially catastrophic overdose.
Years ago, a National Patient Safety Alert advised against prescribing 10mg tablets to avoid this very scenario. Yet, when the OpenPrescribing team turned its eye to the question (see their detailed write up in BJGP) I discovered a hotspot of 10mg prescribing in South East London… right on my doorstep. Suddenly the issue was not abstract any more.
From data to change
The power and beauty of the OpenPrescribing platform is not only that it reveals a problem - it shows where the problem lies. Much of the country had already eliminated 10mg prescribing, but here was a pocket of risk that needed attention.
Why was it happening? The answer varied. In one pharmacy, it was a direct patient request. In another, GPs had little access to specialist rheumatology support. The point was clear: you can’t just issue a blanket warning or run an educational session and expect behaviour to change. You need to understand the local barriers, map the pathways, and involve everyone: commissioners, pharmacists, doctors, and patients.
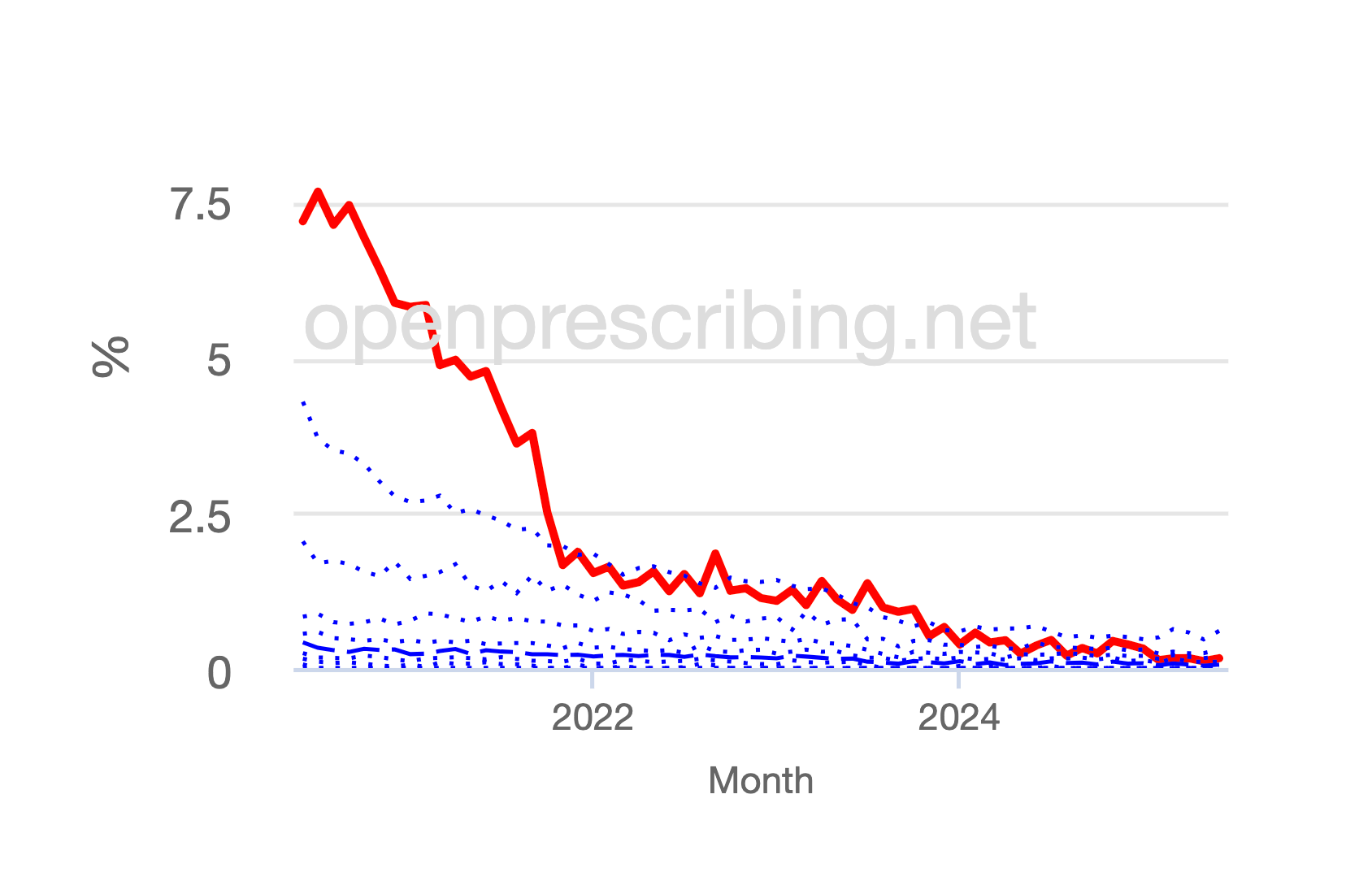
That’s what we did. Using OpenPrescribing we identified where all prescribing was happening, discussed cases and tracked our progress using the intuitive OpenPrescribing methotrexate dashboards. Between 2021 and 2022, South East London went from one of the highest prescribers of 10mg methotrexate tablets in the country to one of the lowest (see chart here). And we were not alone. Nationwide, prescribing practices shifted as a direct result of the transparency and accountability that OpenPrescribing created.
Final reflections
None of this is to say we should slow down the development of new therapies. Innovation in drug discovery remains vital. But we must also match that effort with an equal commitment to using the treatments we already have, safely and effectively, for every patient in every corner of the country.
The real prize in improving outcomes may not always lie in the next monoclonal antibody with a long and unpronounceable name, but in ensuring no patient suffers needlessly from inequity in care.
James Galloway is a judge on this year’s Bennett OpenPrescribing Prize. If you have used OpenPrescribing, like James and colleagues, to tackle an important medication safety initiative in your area you might like to enter. Full details are available at the Bennett Prize Blog.


