OpenSAFELY Service Restoration Observatory: Key Measures
- Posted:
- Written by:
- Categories:

OpenSAFELY Service Restoration Observatory: Key measures for monitoring primary care activity throughout the COVID-19 pandemic
In this blog, we describe the development of a set of key measures used to monitor the ongoing impact of the COVID-19 pandemic on primary care as part of the OpenSAFELY Service Restoration Observatory (SRO). The results from this work have now been published in eLife alongside a live monthly dashboard on reports.opensafely.org.
Changes to primary care during the pandemic
At the outset of the COVID-19 pandemic in February 2020, the WHO issued planning guidelines to support preparedness and response to the developing pandemic. In response to this, the NHS in England paused non-urgent work in hospitals and recommended non-urgent primary care appointments were held remotely. As a result, primary care services requiring face-to-face contact, such as routine blood tests, faced significant levels of disruption.
Initiating the OpenSAFELY SRO
As part of their guidance, the WHO recommended rapid assessments of healthcare capacity and the development of key performance indicators. Early in the pandemic, we initiated the development of the OpenSAFELY SRO with the aim to give an early warning on clinical work displaced, such as cardiovascular disease management; and to monitor services related to clinical impact on patients, such as blood pressure monitoring. As the pandemic progressed, this also gave an insight into NHS England’s goal to accelerate the return to near-normal levels of non-Covid health services, in particular, the aim to “Restore service delivery in primary care and community services”.
Development of the OpenSAFELY SRO
We developed the OpenSAFELY SRO in 3 stages:
Phase 1 - Data-driven approach assessing primary care activity
In the initial phases of the COVID-19 pandemic, it was uncertain which areas of practice would be most disrupted. We therefore aimed to rapidly identify any important changes in clinical practice using a data-driven approach. We did this by producing reports of clinical activity, based on recordings of individual codes within the CTV3 coding system hierarchy, which were shared with a clinical advisory group to identify areas important for monitoring. The CTV3 coding system contains ‘parent’ concepts that describe broad clinical areas and ‘child’ codes of increasing specificity as you move down the hierarchy. We were able to produce reports for individual clinical areas by investigating recording of the most common individual codes under appropriate ‘parent’ concepts.
This initial phase focused on identifying individual areas for continued monitoring within two clinical areas as a proof of concept: pathology tests and respiratory conditions. You can see the results from this phase in our paper, published in BJGP.
Phase 2 - Extending analysis to more clinical areas
Having proved the utility of the data driven approach in phase 1, we then wanted to extend analysis to cover more clinical areas. You can read more about this phase in a previous blog post.
Phase 3 - Developing key measures of activity
Informed by the previous phase, the third phase aimed to create a set of key measures of primary care clinical activity to support routine monitoring, targeted action and inform response to the COVID-19 pandemic. These measures would be comprehensive groups of codes, rather than individual codes, which were used in the earlier phases. The clinical advisory group was asked to suggest key measures for each clinical area considering the following criteria:
- Does it represent a high-volume activity?
- Is it clinically relevant to front-line practice?
- Is it more widely indicative of other problems in service delivery across the NHS?
Phases 1 and 2 were performed using data available in OpenSAFELY-TPP, covering 40% of all general practices in England. In this phase, we extended the analysis to include data from both major EHR vendors in England, TPP and EMIS. This allowed federated analyses and dashboards to be executed across the full primary care records for all patients registered at 99% of England’s practices.
Below we discuss the results of this phase in more detail.
Key measures of primary care activity
We developed 11 key measures of primary care activity, shown in the table below. These key measures include routine blood tests (cholesterol, liver function, thyroid, full blood count, glycated haemoglobin, renal function), reviews for long term conditions (asthma, chronic obstructive pulmonary disorder, medication review), cardiovascular disease risk assessment, and blood pressure monitoring.
| Key measure | What is it and why does it matter? |
| Blood pressure monitoring | A commonly-used assessment used to identify patients with hypertension or to ensure optimal treatment for those with known hypertension, with the aim of reducing long term risks of complications such as stroke. |
| Cardiovascular Disease 10 Year Risk Assessment | A commonly-used risk assessment used to identify patients with an increased risk of cardiovascular events in the next 10 years. |
| Cholesterol Testing | A commonly-used blood test used as part of a routine cardiovascular disease 10 year risk assessment12 and also to identify patients with lipid disorders (e.g. familial hypercholesterolaemia). |
| Liver Function Testing - Alanine aminotransferase (ALT) | An ALT blood test is one of a group of liver function tests (LFTs) which are used to detect problems with the function of the liver. It is often used to monitor patients on medications which may affect the liver or which rely on the liver to break them down within the body. |
| Thyroid Testing - Thyroid Stimulating Hormone (TSH) | TSH is used for the diagnosis and monitoring of hypothyroidism and hyperthyroidism, including making changes to thyroid replacement therapy dosing. |
| Full Blood Count - Red Blood Cell (RBC) Testing | RBC is completed as part of a group of tests referred to as a full blood count (FBC), used to detect a variety of disorders of the blood, such as anaemia and infection. |
| Glycated Haemoglobin Level (HbA1c) Testing | HbA1c is a long term indicator of diabetes control. Poor diabetic control can place individuals living with diabetes at an increased risk of the complications of diabetes. |
| Renal Function Assessment - Sodium Testing | Sodium is completed as part of a group of tests referred to as a renal profile, used to detect a variety of disorders of the kidneys. It is often used to monitor patients on medications which may affect the kidneys or which rely on the kidneys to remove them from the body. |
| Asthma Reviews | It is recommend that people with asthma receive a review of their condition at least annually to check if their asthma control has worsened, which could lead to a greater chance of symptoms and admission to hospital |
| Chronic Obstructive Pulmonary Disease (COPD) Reviews | It is recommended that all individuals living with COPD have an annual review to check if their COPD control has worsened, which could lead to a greater chance of symptoms and admission to hospital. |
| Medication Review | Many medicines are used long-term and they should be reviewed regularly to ensure they are still safe, effective and appropriate. |
Changes in key measures during the COVID-19 pandemic
Most measures showed a similar pattern, with a steep decline in April 2020 during the national lockdown, followed by partial or full recovery over the summer of 2020 and into 2021. The measures for routine blood tests recovered to their pre-pandemic baseline within a year of the pandemic. The recovery of these measures highlights a rapid, adaptive response by primary care in the midst of a global health pandemic. The remaining five measures showed a more sustained drop in activity; asthma and COPD reviews did not recover to their pre-pandemic baseline until around August 2021 and blood pressure monitoring, cardiovascular disease risk assessment and medication reviews had a sustained drop in activity that persisted up to December 2021.
An example of the changes in the measures observed for renal assessment and blood pressure monitoring is shown below.
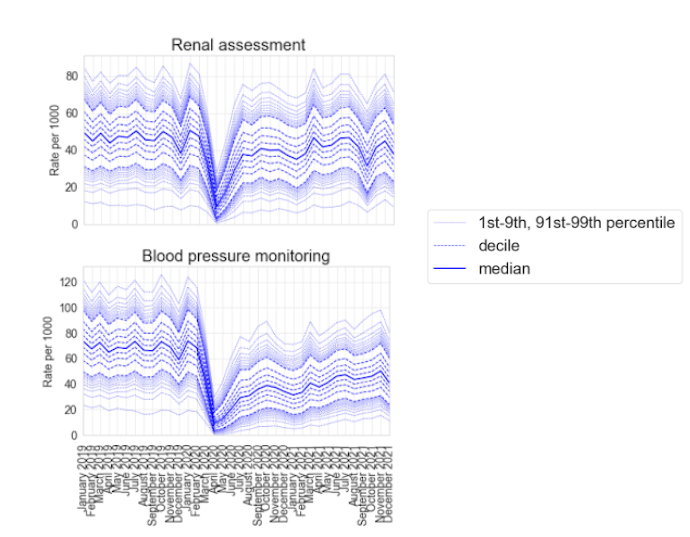
There are many potential causes and reasons for the changes in the measures observed, so careful interpretation is required. Reductions in the measures can represent both changes in volume of activity, as well as changes in the style of delivery of clinical activity. For example NHS Health Checks, which are used to detect early signs of high blood pressure, heart disease or type 2 diabetes, were paused during the pandemic; this is likely to explain the sustained drop in activity in blood pressure monitoring. However, this may also reflect an increase in the number of patients who record their own blood pressure at home, which may not be recorded completely or consistently in GP records.
What’s next?
Reductions, such as those observed, are not necessarily problematic. As part of the COVID-19 recovery, these may represent rational reprioritisation of activity. Where these changes in priority have not been nationally planned, a framework like the OpenSAFELY SRO may help to rapidly identify the pragmatic changes in prioritisation being made by individual dispersed organisations or people across the healthcare ecosystem before those changes are explicitly surfaced or discussed through other mechanisms.
The approach taken here allows analyses to be easily updated, and expanded. We will continue to monitor these changes using our publicly available NHS OpenSAFELY SRO dashboards, which are updated monthly. We can expand on these measures to include any measures needed to support NHS England’s ambition to “build back better” as we recover from the COVID-19 pandemic.


