NHS price concessions cost charities and local authorities an additional £5.6 million last year
- Posted:
- Written by:
- Categories:

In the last year we estimate that price concessions have cost an additional £165 million in unplanned expenditure for Clinical Commissioning Groups (CCGs), and our OpenPrescribing.net price concession calculator was featured in a major BBC news story and in the Pharmaceutical Journal this week. However, interestingly, NHS price concessions do not just affect the NHS: they also represent unplanned expenditure for charities, local councils, and others. Here, we report our estimate of the impact on non-CCG organisations as an additional £5.6 million in 2018: a huge four-fold cost increase on top of expected prices for a sector that is already over-stretched.
What are price concessions?
Briefly: price concessions are a short term agreement by the NHS to pay more than the already agreed price for a generic medicine because pharmacists are unable to obtain the generic at its usual price. Sometimes this is known as NCSO (“no cheaper stock obtainable”) and you can read more about them and the National Audit Office investigation in our previous blog. Here at OpenPrescribing we have also developed useful calculators and alerts to support CCGs and NHS England to monitor the impact of NHS price concessions
Who else pays for NHS prescriptions?
On OpenPrescribing we present prescribing data for all general practices in England. These prescriptions are usually written by staff in general practices, dispensed in a community pharmacy and paid for by NHS organisations called CCGs. This represents the vast majority of prescribing in primary care in England; however, the data we use, published by NHS Business Services Authority (NHS BSA), also contains some information on prescribing by other organisations, where the prescription is dispensed in a community pharmacy. This prescribing is generally paid for by one of three types of organisation:
- Independent providers: These are organisations, such as charities and community interest companies, that provide healthcare related services commissioned by local councils or CCGs, for example medicines to treat sexually transmitted infections. A full list of independent providers can be accessed here.
- Local Councils: Since 2013 local authorities have had statutory responsibility for public health services, e.g. for sexual health and drug and alcohol misuse.
- Hospitals: The vast majority of hospital medicines data is not currently available, but sometimes a hospital prescriber may give a patient a prescription to be dispensed in a local community pharmacy, and some, but not all, of this is included within our normal dataset1.
The mechanism for payment of these other organisations can be complex: local councils sometimes pay for medicines themselves, sometimes they pay independent providers who in turn get charged by NHS BSA and confusingly, sometimes staff in general practices write prescriptions for medicines that are the responsibility of a local authority. In these instances CCGs may pay for the medicines directly and then charge local authorities, but this cannot be determined in our data.
What is the impact of price concessions on non-CCG organisations?
Across all of the organisations that weren’t CCGs for which we have prescribing data, we estimate the additional cost impact of price concessions in 2018 was £5.6 million, on top of the £1.3 million NHS drug tariff cost for these medicines, representing an unplanned four-fold cost increase. Organisations could not have reasonably planned for this additional impact so this would have to be covered from other parts of their budget. Table 1 shows the top 10 organisations with the greatest additional costs from NHS price concessions in 2018.
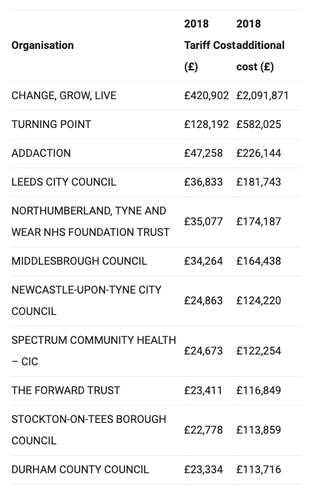
Table 1. Impact of NHS price concessions on non-CCG organisations in 2018
The top 10 drug price concessions are shown in Table 2. It is perhaps unsurprising to see a large impact on the Top 10 organisations as buprenorphine and diamorphine are medicines commonly used in substance misuse services, which are the responsibility of local authorities. There was substantial media coverage of this story (see Guardian article) and some organisations such as Addaction and Change, Grow, Live have written about the implications and how they are dealing with this issue.
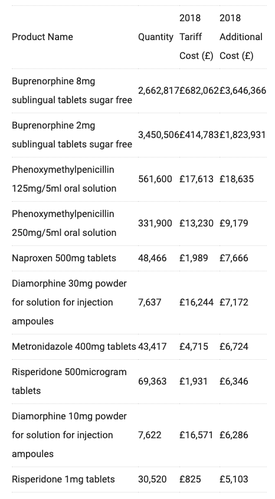
Table 2: Top 10 products with additional cost from NHS price concessions in non-CCG organisations
It is clearly necessary for local authorities and other organisations to monitor the impact of NHS price concessions on their budgets, and we know that many have been doing so. We hope this summary of the impact in 2018 is helpful but if there is anything else interesting that you have found in non-CCG prescribing data please get in touch.
How do you do all this data analysis?
We are a small mixed team of clinicians, academics, and software engineers, pooling all our knowledge and skills to build useful tools and analyses for our users. We think it is unhelpful that so much NHS data analysis is outsourced, or done behind closed doors. We value openness and transparency, because we think open discussion of ideas and methods will help create better insights. So as always, our entire analysis is freely available for inspection, review, and re-use on GitHub, you just need to understand some Python and SQL (if you don’t, then come on the courses we will shortly be running!). Additionally you can follow our discussion on Github here to see how clinicians, academics, and software engineers work together to iterate and solve problems like the one discussed in this blog.
If you would like to see non-CCG prescribing data made available routinely on OpenPrescribing.net please get in touch at bennett@phc.ox.ac.ukespecially if you know of funds that could support further developments.


